My Story, an abbreviated version. For re al.
al.
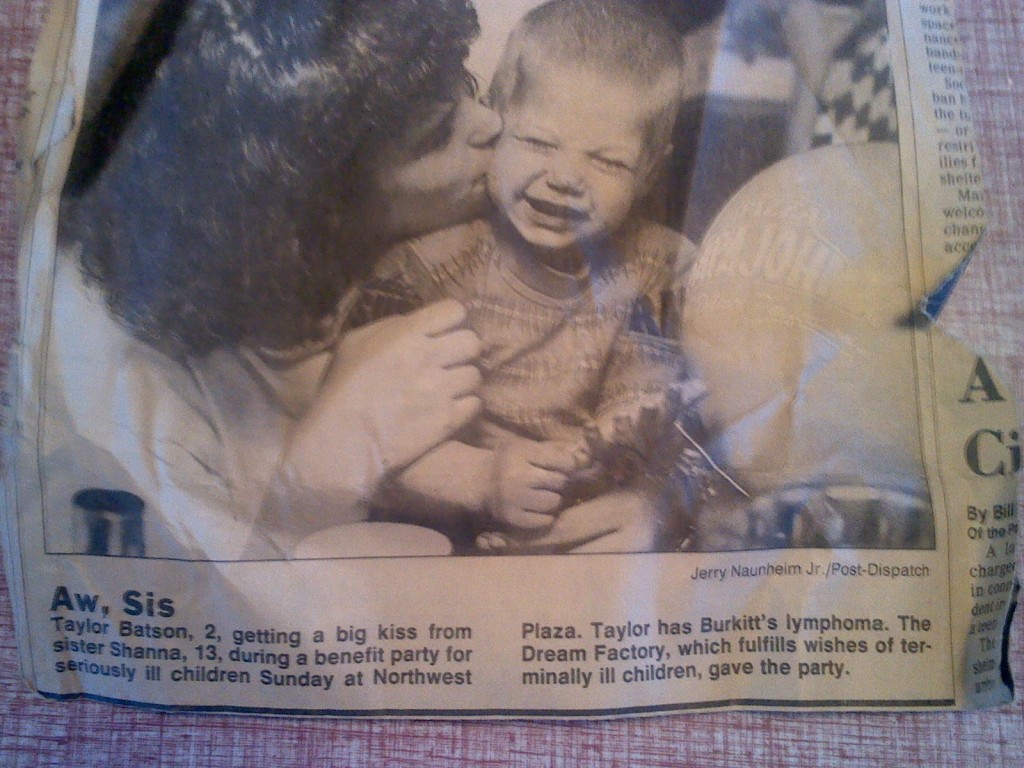
Superman and Captain America. Two strong characters, no doubt about that. These are the nicknames I gave two little premature infant boys I had helped take care of in the neonatal ICU spring 2007. Watching these tiny guys fight for their lives, grow, and go through various trials was routine to me. It was not routine for their mom and dad. I gave them these nicknames for fun. One day the mother asks me why I call Hagan “Superman.” I said, because he had strength he didn’t even know he had.
I became ill January 14th, 2008 on a Monday evening at church. I felt the distinct feeling of the flu: fever, chills, and cold to the bone. The next morning, I felt better and went to work. Driving on I-30, pain began in my lower back. The pain was on the move and increased quickly. I thought I was having a heart attack. I went to the nearest ER and was admitted. 7 days in a hospital revealed I was healthy except for an elevated white blood cell count. No diagnosis was given other than “costochondritis.”
Sickness set in deeply over the next three weeks. I lost close to 30 lbs., became increasingly weak, sweating around the clock, and my pain rose daily. I made several visits to doctors, ER’s, and hospitals looking for help. My symptoms were apparent but the underlying cause remained hidden. I kept working, but had to reduce to half days of work. I was finding the drive back and forth a frightening experience. I couldn’t get comfortable in the car. The level of pain was incredible in my lower back and somehow, the driver’s seat was most uncomfortable. I vowed to never own another car like this again with such an uncomfortable seat! One morning, during the drive to work, I couldn’t continue driving. I pulled off the nearest freeway exit and came to an abrupt stop on the side of the off ramp. I climbed out and began to walk. I walked up the ramp towards the road, turned around, and walked back down towards the interstate. I walked as fast as I could (which was quite slow) and went back and forth, talking with my sister on the phone. I knew something was wrong, very wrong. I wasn’t sure if I was going to have to call an ambulance, as I couldn’t take the pain. After what seemed an eternity, I managed to get in the car and make it to work.
I was referred to an ID doctor for multiple tests: fungal, viral, and other less common possibilities. I was in pain, weak, anemic, sweating profusely, confused, and scared. I was a sick man. She decided I needed a CT of the abdomen, amongst other things. It was one of the few places that hadn’t been poked, prodded, searched, or studied by this point.
On January 24th, I recorded the following:
“I’m still ill. I woke up this morning in a drenched bed. So, this is now my morning routine. Strip the bed and wash it down. Freeze as I’m doing it. I have multiple layers of clothes. Take some ibuprofen. Start the laundry, crawl under a cover on the couch and shiver for about 15 minutes.
Then I feel the chill leaving. I start shedding layers because I know what is coming next. Sweat. I am down to almost no clothes, carrying a beach towel to mop the sweat off of me the last 30 minutes or so.
I can’t sleep much. Fever keeps setting in around 7-10 each night.
Repeat daily.
I tried getting on the computer yesterday, just had no strength or desire to sit in front of the computer.”
February 6th, I recorded the following:
“Still having 24/7 fever, random pains to my back and going into my legs. Tremendous sweats at night. Fatigued.
I had a CT of the chest, abdomen, and pelvic area on 2/5 early in the morning. I received a phone call from the MD office that afternoon. It was one of those better sit down type phone calls. The lymph nodes in my abdominal area are enlarged significantly. Major suspected culprit? Lymphoma.
My dad and his brother have battled lymphoma. I looked up the symptoms for lymphoma online and I’m a perfect match, weight loss and all. Terrible weight loss program, don’t recommend it for anyone.
I’m waiting for the MD office to call with what time they are going to do a CT guided needle biopsy of some nodes in the abdomen. I have not been diagnosed with lymphoma and may have something other. The guy from the office said it was possible for other things to happen that could cause this. I asked him to name one or two….the phone grew awfully quiet….
I’ve cried so much this morning. I don’t feel like it’s my time yet, I don’t fear dying. I do fear ‘having cancer’ and all it entails. The therapies are rough.”
Then it hit me: I HAD CANCER. I knew it wasn’t diagnosed yet, but I had no doubt. I sat in my recliner and let the emotions flow.
Thirty days after my symptoms began, February 13th 2008, I was diagnosed with an aggressive rare form of Non-Hodgkins Lymphoma. February 14th, I was admitted to the hospital to begin chemotherapy. Happy Valentines Day! I was relieved to have a diagnosis, terrified of the possibility of dying so young at the age of 43. I had two teenage daughters, a wife, and a full life to live.
I met my oncologist. He helped me to understand that I had swollen lymph glands all over my body that he could feel with his hands. He asked me if I’d felt my neck lately. I suppose in all the confusion, I missed the rather obvious knots forming around my neck. He stated I would be in the hospital for eight months. Eight (8!!) months. I got a bit testy, as I had to get back to work. Denial at is finest, I assure you. He then said something to the effect that the next 10 days would be critical and I might not make it that long. My cancer was doubling in size almost every day, very rapid growth. I was Stage IVb, advanced lymphoma. A difficult and terrible awareness sank in. I was a man with cancer, confined to a room in a hospital for months to come, now disabled, and I was fighting for my life. Once the gravity of the situation became increasingly real, I broke down.
My nurse walked in and said, “Mr. Baxter, would you like one vial or two?” She sat two vials of morphine in front of me. Thus began my descent into a foreign chemically driven fog. I received a chemotherapy regimen called HYPER CVAD +R, one of the more aggressive chemo regimen that exists. I was to get a total of eight treatments on an A/B cycle approximately every 28 days. I watched various colors of fluids drip into my veins. I would have to drop steroids into my eyes on the “B” cycle to prevent corrosion in my eyes from chemo being secreted into the tear ducts. Bone marrow biopsies, blood product transfusions, frequent lab draws, being awoken every 2-4 hours for vitals or a medication, and so many unexpected twists and turns took away all control I had. I was at the mercy of the medical system, which was responding to my unpredictable and severe illness.
Maybe about one week after I was admitted, I found I was eating my food and the texture seemed wrong, rather odd. I hobbled across the room, dragging my IV pole, and looked in the bathroom mirror. Blood. I had been chewing on my bottom lip and could not feel it, not at all. I had absolutely no sensation in my lower lip and lower jaw. I had chewed on it enough that the doctor informed me the next day a soft diet and feeding tube were in my future if this continued. I quickly adapted and learned to not bite the bottom lip. I became used to the sensation of cold water running down my lower lip and chin, evidently a trick of the nerve endings.
A neurosurgeon said I had a decision to make. Did I want frequent spinal taps to instill chemo into my spine (less effective) or an “Ommaya” Reservoir in my scalp for a more effective infusion of “intrathecal Methotrexate?” I had never heard of an Ommaya Reservoir in many years of being an RN. It is a port to the brain. He explained he would make this small semicircular incision on my scalp and place a small flexible tube through my brain into the opening in the center of my brain. I responded, “You didn’t mention you would have to drill a hole through my skull.” For the record, I have a rather profound aversion to anything being done with my teeth or bones. He deftly replied, “the drill has a clutch in it so that it will stop spinning as soon as it pierces through the bone so it doesn’t nick the grey matter of the brain.” When I told my dad what the surgeon said, dad wisely cracks “hope the clutch don’t slip.”
Thanks dad!
The insertion of the Ommaya Reservoir occurred, spent 24 hours in the neuro ICU, and finally woke up early the next morning in the neuro ICU. I had been out for the better part of 20 hours. One surgery and CT scan later, I returned to my oncology room with a sore scalp. I learned quickly to not lift my eyebrows; not smart at all. These are the muscles that go across the scalp, right where they put the Ommaya.
The nurse comes in that evening, rather late, and states “Mr. Baxter, you’re scheduled to return to the operating room early in the morning.” I lifted my eyebrows when she told me that! I was not a happy camper. Evidently, the Ommaya tubing was not in the optimal position. The neurosurgeon came by later that night. “Hey doc, not too happy. You owe me an Ommaya set up so I can show my students. That’s the cost of having to do the same surgery over again.” Hmmpf. Another trip around the hospital for revision of the device, another CT scan, and I was back in my room with a really sore scalp. I assure you, I did not lift my eyebrows or laugh for a short while after that.
Insertion of the second PICC line was eventful. Specialized RN walks in, introduces himself and explains the procedure, and proceeds to set up the equipment on my right. That put him and his toys squarely between the bed I’m lying in and the door to the room. He walks me through the process and does a nice job. He leaves, stating the x-ray machine will arrive shorty to confirm correct placement. I hop up and decided to give dad a call. I’m using my right hand, the arm with the new PICC line, to hold the cell phone. I walk around the room, pacing a bit. After a few trips to the door and to the back of the spacious room, I noticed drops of blood on the floor. It was near where he had inserted the PICC line. This thought crosses my mind, “he didn’t clean up some of his mess.” I kept pacing, talking with dad. I found myself stepping over a few rather large blotches of blood on the floor. This went on for a few more minutes. I finally told dad, this guy made a real mess and didn’t even bother to clean it up. I kept slowly pacing around. It was becoming harder to step over the blood as there were few spots where I could put my socked feet and not step on blood. I finally stopped the conversation with dad and told him with a bit of aggravation, “I can’t believe this guy, he created a mess all the way from the front door to the back of the room.” A chilling reality hit me: he never went to the back of the room. Where was this blood coming from? I stood still for a moment and studied my legs, nope they are fine. I saw it happen! A big drop came off from my right elbow. I looked at the clear plastic covering over my PICC line and blood was steadily flowing out, down my right elbow, and dripping on the floor. I said, “Dad, I’ll have to call you back.” It was probably only a moment in time, but it seemed like an eternity. I looked across the room and saw red glistening across the floor. It was rather impressive. I, umm, well not really panicked, but sort of. I called for the nurse and lifted my right arm up high, holding onto the IV pole. I stood there and realized I had not felt the blood dripping down my arm and dropping off my elbow. I found that odd. I couldn’t feel it. How could I possibly not feel blood dripping down my body like that? I got a bit upset as I saw how much blood I had lost. I’m sure it wasn’t as much as I felt it was, but seeing that much blood spread around the floor was rather startling. God bless that kind nurse that got on her hands and knees to clean up all that blood!
I could have never been prepared for what was to come: lack of sleep for months, constant monitoring of the blood, replacement blood products, various stages of chemo agents, trembling, ears ringing, sitting for untold hours staring at the same hospital walls, weakness, and atrophy of my muscles. The journey becomes convoluted, unpredictable, and intense, with significant highs and lows. Days and nights blurred together. Chemicals of all kind were put in my mouth, in my veins, and in my central nervous system. I ended up with an Ommaya Port placed in my scalp, PICC line in both arms (one at a time), eventually got a double lumen port in my chest. I was warned my hair would begin falling out around day #21. I decided I couldn’t do the patchy look so I had my family shave my head. I discovered “steroid rage” was a very real phenomenon after taking massive doses of steroids twice a day.
The chemotherapy “to my brain” (as I put it) caused painful side effects. I discovered this when getting out of the hospital bed one morning. Ever been in a car that had windows that seal too tightly? It will compress the eardrums of everyone in the car as the windows shut. Not fun. That was the warning I felt that meant I should sit down and get ready for a head banging time. First the eardrums move, feeling as if they were sinking in. Then the head throbbing would follow. Add in a touch of dizziness and that was my recipe for a skull full of pain.
I want to share what happened after my third dose of chemo. I was supposed to go home April 22nd. I recall being awoken and sat up in bed. One person on my left was talking to me saying something. I was sleepy, really drowsy, and fell backwards to sleep some more. This is significant in and of itself considering I was normally awake and having trouble sleeping most of the time. I recall being sat up again, the feeling of gentle slapping on my hands and my face. This time there were two people, a nurse was now on my right also. I could register some voices saying, “Mr. Baxter, you need to wake up, wake up now.”
I felt like a limp boiled noodle. My neck was weak, my arms and legs had no strength to them, and I was wanting to do was to fall backwards in bed to sleep. They wouldn’t let me. They forced me to sit upright and kept talking to me rather excitedly. I tried to focus my eyes and saw too many people in my room. People were moving around quickly; the door to the room opening and closing several times. I mumbled something to the effect “I’m so sleepy, let me sleep.”
The voices stated again, “Mr. Baxter, you have to wake up, now isn’t the time to sleep.” I got a bit irritated, but something registered inside my head that people moving quickly in my room trying to wake me wasn’t normal. When medical staff move that fast, there is usually a good reason. I tried to force myself to focus. It was hard. I felt so doped up, so weak, almost distant from my own body. I didn’t have much sensation, no particular pain, no nothing. It was almost like I was alive consciously, but my body wasn’t attached to my brain. The lack of sensation was hard to describe. I felt peaceful. I wasn’t feeling the usual sensations of chemo sickness, no headaches, no bone pain, actually I felt rather blank.
I managed to ask what happened, why are so many people in my room. The patient care technician to my left explained she came in to take my routine 4am vital signs and I wasn’t awake. She knew something was wrong. I rarely slept. If I were asleep, I was easy to wake up. She said I was sleeping soundly. She proceeded to count my respirations and couldn’t see me breathing. She got my pulse quickly and found it was 32 beats per minute. She called for help, hooked me to the blood pressure machine, began to try to wake me, and I wasn’t responding. My blood pressure was something like 68 on top and didn’t register on the bottom number.
My brain was catching on that something wasn’t right. I mumbled 32 isn’t a good heart rate. She said they had drawn blood and were waiting for results. They were thinking it was potassium related. They kept me talking to me, asking me questions. I started dozing back off. I could feel sleep coming on again. I couldn’t fight it to save my life. I was sliding down and they were sitting me up, telling me I “had to stay with them.” I could tell by the urgency in their voice they weren’t messing around. I’m not sure how long this went on for, but it lasted a while as they scrambled to intervene.
I eventually started feeling the strength to wake up, the desire and ability to make some effort to do anything but sleep. The same pct was still next to me, talking to me, encouraging me to sit up and interact with them. My potassium had come back at 2.7. That is low enough to slow down the muscles and nerves in the body, essentially suppress my person. They had given me an infusion of potassium IV. It was helping. The slow reality that I had come close to death was creeping into my soul. I started to give my all to staying alert, trying to talk, anything but not sleep. I wish I could say I felt fear, but I didn’t. It was so peaceful.
As the night turned into morning, my wife arrived. I recall the nurses and techs coming into my room every few minutes and making me answer questions. I recall them telling my wife she had to keep me awake. I was still drowsy. I was now short of breath, and sweating with the slightest exertion. The symptoms worsened as the day went on. They performed an echocardiogram and determined I had developed a large murmur in my heart. I was told mine was classified as prominent. I was moved to the telemetry unit and told I was ‘throwing some PAC’s’, which means my upper chambers of the heart are beating out of sync with the lower chambers of the heart. Again, this can be potassium related.
Telemetry brought about many changes. No more cell phone use. The unit was very, very old. The room was so small that I could hardly move the IV pole. I would get out of bed, walk in a half circle around the IV pole that was just to my right, and be at the bathroom door which was about 5 feet from where I slept. The bathroom is so tiny I had to leave the IV pole outside the bathroom. I could barely close the bathroom door when I was in the bathroom. My left elbow would touch the sink and my right elbow touched the old fashioned bathtub. Ugh. Very different from the beautiful suite I’ve been in so far. This unit was the last remaining units in the original old building. It was a throwback to days gone by. Cinderblock everything, few conveniences, and to take a shower, I had to use a community “shower room” down the hall. Awkward to say the least. No windows to look out of and nothing to help ensure a positive attitude. I felt I was in a jail. At night, I was staring down the hall. I could almost envision Florence Nightingale walking down this hall. No internet, TV was poor, and I was trapped in that small room. I did more walking in those few days in telemetry to keep my sanity than all the previous hospital admissions combined. I found myself becoming depressed and slipping closer to despair. I wanted out. That was a very difficult time for me.
The physical environment was rather oppressive, just the opposite of the oncology ward. Everything was small. There was a musty smell in the air. The corridors where smaller and darker than newer hospital wings. The ceiling seemed lower. They didn’t have any waiting area or place for anyone to sit in the hallway, unlike the oncology floor. Nothing was bright or cheery. Honestly, it was depressing.
Many nursing students seemed to be flooding this ward. I don’t recall that many, if any, on the oncology ward. I was a subject of curiosity for them. They wanted to touch my Ommaya reservoir and see the double lumen port in my chest. I made the highlight of one student’s day when he got to access (put the needle in) my chest port. Oh boy, pin cushion Robert at your service, let me tell you. They each wanted to come in and ask me about my complex medical history.
It was during this time when I had one of the two episodes where stomach contents met the floor. No warning, just a 2 second sense that my stomach was upset. I was again impressed at the ability of the human body to eject contents. I called the nurse and they told me to get in bed and stay there to rest a while. Most curiously, once done, it was over. I didn’t have any gagging or lingering sense of nausea. I was grateful for this small concession, I assure you.
I measured my progress by my heart rate. They would come in to check on me frequently. I would ask my heart rate. “in the 40’s.” “in the 50’s.” When I finally heard that my heart rate was in the 60’s, I rejoiced. I later found out my heart was still going into the 40’s at night when I was asleep and this concerned me. I commented to the cardiologist I needed to eat more bananas. He said to not worry about it, commenting that bananas were not a rich source of potassium like people thought. Yes they contain some, but much less than is popularly spoken. When they weren’t in the room, I would reach over and pull out my Morten Light Salt that I had managed to acquire. Light salt is mostly potassium chloride mixed with a small amount of sodium. When I got home, my wife made sure I had plenty of Gatorade to drink.
When I was told I could go home from telemetry, a circus started, one I knew too well as an RN. The cardiologist said early in the morning I could be released. I asked the nurse to contact my oncologist right away. I was so ready to get out of there I was nearly desperate. No go, he’s not working today. Great, I have to deal with an on call doctor. That always means a “manana” attitude. Sure enough, “well the doctor said he’d be in to make rounds later tonight.” I sat there all day. My despair was turning to anger, feeling like I was being held for no reason other than convenience of another person. By eight pm, I was livid. I assure you, my heart rate wasn’t low at that point.
The on call doctor makes rounds and says “go home.” Oh boy, he had to walk in the room to tell me the obvious. My wife had been at work since 4am, it was now after 8pm, and I had no ride home. She was still at work. I pressured the nurse to get something done as I didn’t want my wife having to come pick me up at 10:30 pm after working 16+ hours of hard work. It was a long drive and a long walk. They finally told me that “NETI” would come pick me up. Sure enough, some EMT type of set up arrives. Onto the gurney I go. I am placed in a van with my head by the drivers seat, lying on the gurney, looking at the ceiling of a van. I can see the interstate flying by. It was a bit nauseating. I finally figured out they were taking some long way around to my house. I didn’t have the strength to say anything as I was focusing on not being ill. I finally arrived home and they allowed me out of the van. I had to sign release papers. Then something odd happened. The walk up the slope of my driveway to my home was long and hard. I wanted to fall out right there. It isn’t but maybe 30 feet from the curb to the front door. I stood at the door and realized I didn’t know where my house keys were or if I even had them. I realized I didn’t even know where my wallet was. I had this short moment of realization I hadn’t seen my personal belongings in who knows how many weeks. I felt a twinge of loss of control at that moment, standing by my front door, not even sure how to get it. I had to dig through my gym bag and eventually I got inside. I was met at the door by one of my daughters who had made a sign that said
“welcome home dad.” Indeed, glad to be home!
Little things took big importance. For example, sitting in a recliner became painful. Trying to get comfortable in the recliner took several pillows and a few minutes of adjusting. Walking became quite a challenge. I attempted to walk around the nurse’s station only to discover it would take hours of recovery time after only a few short laps. Didn’t see the point in that. I got to watch the hospital complete an expansion and observe with mild amusement (what else did I have to do at 8pm on Tuesday evenings?) the hoopla of the opening ceremonies with a bird’s eye view through a window from the 7th floor. I never knew I could value regularity so much. I endured extremes of diarrhea alternating with constipation. Sweet little dietitian would visit weekly about protein levels dropping. There wasn’t much to say about my diet as the food source didn’t change from day to day. Chemotherapy even affected my need for eye correction. My vision changed so frequently that one day my glasses would help, next day I didn’t need them. Other days things seemed blurry with or without glasses and I just didn’t have the strength to care.
Relationships became more important than ever. Cards and books and so many kind gifts and thoughts kept flowing into my room that it was overwhelming. The support being shown was tremendous. Friends from childhood all the way to present supported me. My mom and stepdad were regulars, sacrificing time and money to stay with me as much as they could, especially in the beginning when so much confusion was present. Each person who visited, the generosity shown by family and friends, by my parents and Janice’s family, by my daughters, was fuel to help me keep going. Every time I received another act of love, it was powerful to me. I’m not sure I conveyed it well, but I did feel the result of every choice each person made to honor my family and I; every act of kindness increased my resolve to make it another day. I received phone calls from relatives I hadn’t spoken to in a long time and felt so much love and support. Family gave their all in physical ways, financial ways, emotional support, the sacrifice of so many was touching to say the least. I had people from present and previous jobs showing up to visit and sending cards. I got a notice the fence in the back yard had blown down. A few days later, I get a picture of my next door neighbor laying in my back yard with a cement post across his chest. My daughters thought that was cute and sent it to me.
One day, two ladies appeared with their toddlers in the room. These were infants I had taken care of in the neonatal ICU two years earlier. Parents of these boys found out I had cancer and came to visit me. I found that profound. They stayed a while and the room emptied of some other visitors. Dad and I sat there talking with them and I had to ask how they heard about my cancer, as I was not in contact with them or my previous work. They had heard from someone that I had cancer, seems news was spreading fast. I asked them when they found out. The response? That same morning, just a few hours earlier.
I sat there in disbelief. I was blown away by their kindness in coming to offer me and my family support. My dad was standing to my left, I was sitting, and they were standing in front of me. I mentioned I was so touched you would come to see me. I find it more than generous and has certainly caught me by surprise, means so much to me that you would care that much. They said something that has had lasting impact on me. They shared how much I had meant to them during the trials they endured when their sons were born. They said I meant so much to them. Keep in mind, I do recall them and their stories. I recall taking care of their sons for many nights. I do not recall doing anything out of the ordinary for them that I would be deserving of such an act of kindness. I said so, too. How was I different than other nurses who gave excellent care?
They said something I won’t soon forget. They said I had given them hope when they felt they had none. What I thought was a routine night shift in a NICU, they saw as someone who cared for them and their son. They said they slept well at night when I was there. They mentioned other nurses that provided the same comfort to them. They felt hope and good things coming.
They wanted to do for me what I had done for them.
I lost my man card at that moment in time. I lowered my head and the tears cut loose. I had no idea I had meant so much to them. Time slowed down at that moment for me. I was so overwhelmed at their words, their kindness, and generosity. I told them so. They said it is the least they could do for me. I can see my dad’s right hand reaching to his back pocket. Out comes the red-checkered handkerchief. H-O-N-K goes the nose. Dad gave up his man card too. I took away from that moment that one never knows the impact they can make on another. What may seem routine to one is a moment of hope to another. Acts of kindness can go a long way and are so refreshing when returned.
Family members brought us help and hope too. The first thing to mention about our family is that we are a geographically diverse family. My wife and daughters and I live in North Texas. Our families on both sides are spread out over Texas and New Mexico, most of the distances being long. We were by ourselves. The reality that they would sacrifice so much to drive so far to help us was deeply touching. So many came up at varying times and helped our daughters by taking them shopping for school clothes. Some came up and fixed things around the house. Some came up and cooked food and stored it in the freezer or sent us food through various merchants. Our daughters didn’t have cell phones so they were given “go phones” covered with sparkly stuff. My stepdad bought me a laptop as he said he knew I would go crazy sitting there for 8 months with no outside contact. My daughters watched movies with me, snuck down to the cafeteria with me to get “real” food, and did various neat little things to lift my spirits. My wife brought me food, real food, junk food, good food, anything but hospital food! She brought me Starbucks and was so kind to me. I know I’m forgetting some things that were done; the generosity was so frequent and so powerful. Please forgive me if I don’t mention your act of kindness.
One of my daughters made a bright pink poster to put on my hospital door. It read:
“My doctor says it is not the cancer that will get me. It is the germs on your hands. Please come in and wash your hands.”
I put that bright pink poster on the hall side of my hospital door every hospital stay. Yep, brought it with me and took it home every time. I could always tell when a new doctor was coming into my room. The door would open partially, I could see this white lab coat standing there reading the sign, then they would come in smiling saying “nice poster.” Months down the road, I was walking the hallway and a lady and I struck up a conversation. She commented about how the young girl has been here a long time. I asked her which young girl? She said the one with the bright pink poster that moves from room to room. I got the pleasure of introducing myself as that young girl! Funny true moment.
As I prepared to go home for my first time, the image of the front of the house flashed through my mind. I made a focused effort to picture the front door, the flowerbeds, seeing my daughters, and remembering what it was like to be at home. I had truly forgotten those small things as the weeks in the hospital labored on and chemicals layered one upon the other. As I realized I was going to finally return home for my first visit, waves of emotion overwhelmed me at just the mental image of my home. I hadn’t got to see my daughters much and missed them terribly.
I did not realize how hard being home would be on the family and me. I had become use to a routine, always having help at the push of a button, food brought to me, and having someone there 24 hours a day to tend to me. I didn’t have to think for myself when in the hospital. The first night at home it snowed and iced over. I couldn’t sleep. I walk in a daze to the bathroom. Seeing myself in that large mirror, late at night while the house was dark, I saw a pale weak man. I realized I hadn’t seen myself much as standing was difficult and the mirror small in the hospital. The home mirror was huge and I could get a really good look at myself. This pale swollen bald man was staring back at me. It was overwhelming to take in fully how bad I looked. I looked sick and felt that way. I ambled slowly to the living room. I sat in the recliner relishing the feel of it, tried to enjoy the TV, but found I could not focus for long on anything so I turned it off. I sat looking around the house. I couldn’t sleep and watched the snowfall, realizing my wife would be awake in the early morning about 2:30am to go to work. I tried to warm the car for her and that was a bit of a disaster. I broke the windshield wipers and broke the fan in the car heater. I did all that with very little effort too. Talk about confused.
I felt gratitude for being at home, followed by moments of confusion and fear. I was unprepared for taking care of myself when the family was gone. I got frustrated over feeling this way, as I had never considered before what it would be like to be so sick that simply getting food would be a chore. The house was quiet. My wife was at work and daughters at school. I realized at some point I needed pain meds and slowly lumbered back and forth to get them. I was shocked at the effort it took and how tired I was. The pain was not good. I realized I couldn’t get up to get anything without considerable effort and decided I couldn’t move much until the pain medication kicked in. I made sure I had a phone beside me and I tried to sleep. Sleep did not come. I sat for a couple of hours waiting for the medication to take effect. Eventually I got hungry and saw the refrigerator across the room. Suffice it to say, the things I took for granted: preparing food, getting a drink of water, basic needs, I no longer took for granted. I went from a state of dependence on a system in the hospital to independence while the family was gone. Real world scenarios don’t always allow for a caregiver to be sitting there to help me nonstop. I was so out of it that I missed that it was my youngest daughter’s birthday. Did not realize it until they had a cake brought out and were getting ready to sing happy birthday. I was so angry with myself when I realized I didn’t even know it was her birthday! Anger mixed with so many other emotions, yet feeling so happy to be at home. I was a mess.
I made it 4 days at home and it was time for my first oncology visit. I was rather exhausted that morning. Seems I was getting weaker by the hour. I was out of breath going from the bedroom to the recliner, a distance of about 30 feet. I couldn’t reach down to tie my shoes. It was a moment crystallized in my memory when I had to ask Janice to tie my own shoes. I was so tired, more so than ever before. I made it to the car and rested. From the car I made it through the sliding doors and found the first bench. I sat and waited, catching my breath and gaining strength to make it the next 20 or so feet to the elevator. From the elevator, I got to the front desk about 40 feet away. I held onto the counter and the lady asked me to have a seat. She could tell I didn’t feel good. Before I knew it, a nurse was at my right side with a wheelchair asking me to move to the wheelchair. I was zipped to the large infusion room in back. My blood pressure was taken and it was something like 86 over 30. They put my feet higher than my head and began infusing fluids. The oncologists face appears, hovering over mine. He said I didn’t look well and needed to be hospitalized. On to the hospital I went for my next stay, a few days early.
Thus began a rhythm of ups and downs, advances and retreats. I was in and out of the hospital. I would go to the oncologist’s office. Then go get units of blood and platelets. I found after the blood transfusions, I would have temporary energy boosts. When I felt strong enough, I would go run a simple errand. When I first got behind the wheel of a 2,000lb metal machine with wheels, I wouldn’t let it go much over 20mph. Other drivers didn’t care for that. I realized I had to speed up; going 30-35 mph felt like I was flying along. I was scared to drive for my first time since I was 16 years old.
I had no idea how bad public outings could be. Let me tell you something, the human body is quite capable of tripping up its owner and that reality became my reality. It was terrible. I couldn’t pinpoint that strange odor in Best Buy. The isles become long as I slowly walked to find the restroom. A new level of shame over my inability to control my own body emerged. What to do in a stall in a technology store with just my clothes on my back and I no longer wanted to be in public? Survival at its finest. How do I exit gracefully in a situation like that? I discovered the human nose is capable of discharging, without one moment of warning or any sensation whatsoever, an impressive amount of clear thin watery solution down my shirt, right in the middle of Albertsons. It happened while standing in the bread isle next to some random person who got the joy of witnessing damage control. I wasn’t ready for something like this, had never had it happen before, and the amount of liquid was impressive. I didn’t know what to do so I grabbed my shirt and tried to contain the flow. It was a real mess. It happened again while checking out at the register at Radio Shack. I’m finishing my purchase when my ears start the deep movement. Here comes the head pounding. Then the nose gives no warning, just a huge watery release that I couldn’t contain, predict, or manage. My shirt was soaked and I learned to simply suck up the shame and keep going. I was humiliated. I focused on walking, just walking ahead and concentrating on making it in full retreat to hide in the van and rest.
When I got home after one long hospital stay, I was handed a rather large box. Inside were various cookies, puzzle books, and many great gift cards. I found this large yellow duck that would sing “splish splash I was taking a bath” when the stomach was pushed. Then I found a picture frame with two pictures in it. It was me holding one of the preemies I called “Superman.” The top most picture, his eyes were closed and he was surely tiny and weak. The bottom picture, his eyes were open, his face filled out a bit more, and he was certainly sporting less tubes and looked a bit stronger. Oh my gosh, this box is from the family of the twins I helped with! It’s from Superman and Captain America! My daughter said the mom had dropped it by the house, hoping to see me. I was sorry I missed her visit.
The box was big and deep. It has so many great treasures in it. When I got to the bottom, I found what was to become perhaps one of my finest treasures of all. Folded neatly in the bottom was a faded blue shirt. I unfolded the shirt and beamed with pride when I saw it was a Superman shirt. I noticed how the Superman logo wasn’t slick and shiny as is typical, but rather, it was scratched, worn, cracked, and appeared to have been through a terrible battle. Wow, Superman must have been in a terrible fight! It wasn’t the usual slick cool looking logo, but rather, a beaten up Superman look. I noticed a piece of paper pinned to the shirt. I unpinned the paper and opened it. A line was drawn through the middle from left to right. Above the line it read
“Remember how you used to tell Hagen he was like Superman? How he had strength he didn’t even know he had?”
Below the line were the words:
“now it is your turn.”
Words cannot convey how hard that hit me. I couldn’t stop marveling at the impact of that one sentence. Took me a while to stop crying. My man card flew out the window at that moment. How in the world did they find out? Oh, I didn’t care; I was elated over that shirt! After that moment, I wore it most of the time I was readmitted to the hospital to remind myself I had strength I didn’t even know I had. That one act of kindness made such an impact on me. I try to retell this story from time to time, but have to be careful. I cannot share it without my eyes sweating something fierce.
I was told I would not sleep much during chemo. They were too reserved with their words. The degree of internal trembling and pure energy that shot through my innards and bones is difficult to describe. Nights blurred into days as the sterile environment of the hospital merged from one set of vitals to the next lab draw. Nights at home were quiet and I would get tired of lying around so I’d amble about. I had trouble focusing enough to watch TV or a movie, didn’t feel up to getting on the computer often, there wasn’t much I could do. The chemicals and sickness took their toll and I know I was confused more than once.
I awoke very early one morning at the house, lying on the floor of the living room. It took me a while to figure out where I was and why I was there. I saw CD’s and items that had previously been stacked by the TV scattered around where I was laying. I wasn’t sure why DVD’s were laying on my chest. I slowly got up and looked around. Things were scattered around on the floor. Something sharp was stabbing me in the back of my shirt. I reached around and pulled out from my shirt about a 1-inch piece of wood, dark thin wood. I sat there trying to figure all this out. Last I recalled, I was lying in the bed and then I was on the floor. Evidently I had meandered out of the bedroom, knocked over a lamp, fell onto a wooden magazine rack and broke it. This caused a piece of wood to lodge in my shirt. Then I estimated I must have made it to the TV to do something and fell out across the floor knocking over items stacked next to the TV. How long was I out? I had a faint memory of trying to pick up a magazine and sliding down the wall instead. I couldn’t read so I must have gone to the TV. After I pieced all this together while sitting on the living room floor, I knew it wasn’t a good scenario to be that confused. I was a bit nervous after that, fearing what would happen to me due to chemicals and insomnia.
By August I was exhausted and weary of the entire regimen. I had had a really trying weekend. It hurt to sit in the bathtub. No meat on my bottom. I got so weak either Saturday night or Sunday night I wasn’t sure if I was going to be able to get out of the tub. That was a scary moment for me. I was so weak I couldn’t stand and I was afraid of slipping on the tub floor. I spoke with my wife and she encouraged me to go to the emergency room. I felt I had an ounce of energy left in me and decided the ER could wait. I have my routine oncology appointment Monday morning and I can make it until then. I did get a little stronger a few hours later once I managed to slowly climb out of the tub. I decided I could no longer take a tub bath, too dangerous and difficult.
Monday morning came. Janice checked on me before she left for work early in the morning. I wasn’t feeling good. I had this belief that going through chemo felt terrible and this was part and parcel of the ordeal. Feeling bad was normal. I told her to go on to work and I would manage. I mean, what was I to expect, to feel good? What I did not realize but can see looking back, I was reaching one of my lowest points and had no business being at home. Easy to see that now, but hard then. I felt about as bad as I thought a person could possibly feel and still be alive. I kept telling myself chemo is rough, what more could I expect? I certainly wasn’t supposed to feel good going through chemotherapy.
I knew it would be an exhausting long day of office visits. Usually meant blood transfusions, too. I stood in my closet and decided it was time for the Superman shirt to help me out. I needed some strength. The family was at school and work. This was after chemo round #6 and before #7 was due to begin. Drying off after the shower, I noticed I had a bruise on my bald scalp. I didn’t remember hitting my head on anything. I put on Superman and got medications I might need for the day. I walked slowly to the refrigerator and got my lunch. I got my salty crackers and my thermos of super salty chicken bullion. I had gotten in this habit of bringing my salty stuff with me after that super low blood pressure scare my first time at home. I slowly walked to the car. I noticed more bruising when I got to the car. Odd. I slowly drove to the oncologist’s office. I recall that drive. It was one of the longest I had ever made in my life. Time seemed to slow down. I inched along every block wishing I were already there. I felt sucked dry of every last fiber of energy. I was determined to press on. I almost didn’t think I would make it as I felt about as bad as I had ever felt. I could not imagine feeling much worse. I was beginning to realize I should have listened to my wife and gone to the emergency room a couple of nights earlier.
I arrived at the oncologists office and sat in the car to rest. It was a good walk of 200 feet or so to reach the front door. I walked from the car to the first bench, about 100 feet. I sat in the sun for a while, feeling it warm my skin. I wasn’t sure if I could make it much further. I determined to press on after a bit and forced myself to walk. I shuffled very slowly through the doors and sat at the bench just inside the doors. I got to the office waiting area, stopping at each bench along the way to the front desk. Texas Oncology is a large place always full of people moving here and there, waiting in one area or moving to the next. I had experienced this before: extreme fatigue, stopping to rest every 20 feet or so. Yet somehow this felt different, even worse than I could recall. I eventually got to the second waiting area. I found that I was so focused on making it, on walking to the next place, that I was almost drawn deep inside myself. My hearing, for whatever reason, seemed unusually strong. Best way I can imagine saying it was like all my senses were dulled except my hearing. I heard two distinct comments, words that have stuck with me to this day like “bless his heart”, and “remind me I have nothing to complain about if I ever get that bad.” I could tell they waited until I was a little distance from them to make their comments, but my hearing was really strong at that moment. I sat in the chair and felt my last ounce of energy melt away, simply gone. The noises around me became a blur of sound.
Most chairs in the waiting room were full. The one to my left was empty. I closed my eyes. Rest, finally. What a long exhausting drive. The walk had finished me off. I could tell a nap was in order. I began slowly tilting to my left. I wanted to sleep and didn’t care if I looked a bit off kilter. I felt myself slipping into a nice needed nap as I relaxed. It was a slow maneuver as I sunk deeper into my own bubble. I felt strangely comfortable, almost like warmth on my left ear. I decided it mattered not and decided to just go to sleep. Eventually I came to rest on someone’s shoulder. Ahh, warm and comfy. I believe I do remember thinking how I am resting my head on someone’s shoulder, a person I don’t even know. I actually did not care and made no effort to sit back up or speak to the person. I drifted into a sleepy mode at last and the world seemed to shut down.
I heard a voice speaking softly. Eventually I realized it was talking to me sayin, “Mr. Baxter, why don’t you come on back. I think we’ll get you in quickly this morning. You aren’t feeling well, are you?” I could tell it was the shoulder to my left. I found this curious as I was sure I had been asleep for a while. I mumbled, “I’m so tired.” It was one of the nurses. She had sat next to me. My head was heavy and I labored to lift my head up straight. I shuffled rather slowly with my head down. The walk was long through a waiting room full of people. It was now quiet and I could feel everyone staring at me. Someone had notified the staff there was some sick man in the waiting room and I was now the center of their attention. I was acutely aware of this. Superman was out of strength.
They normally weigh me as soon as I make a right turn in the door. She didn’t stop me at the scale this time. She sat me down in the first open exam room. I felt something wet on my face. The nurse was handing me towels. It all seemed to be in slow motion. I wiped my nose. Blood was on the towel. I proceeded to wipe again. More blood. I could feel dripping. More dripping. More blood was on the towel. I could feel this steady dripping and held the towel under my nose. The reality of the entire last few days, of the last few months, was setting in harder than ever. The reality of everyone staring at me in the waiting room hit me. The long drive, the hard walk, unable to tie my own shoes. All of this seemed to crystalize that one moment.
I realized I was spontaneously bleeding from my nose. I could see bruises up and down my arms and legs. This deep well of emotions started to pulse in my stomach and chest. I felt helpless, weak, and humiliated, absolutely humiliated at what I had become. I looked up at the nurse. She said, “We’ve already called the ambulance, they are on their way.”
I lost my man card at that moment. Again. In a Superman sized way.
I could no longer control anything. I couldn’t control my emotions. I couldn’t control my future. I couldn’t control where I went from day to day. I couldn’t control bleeding and bruising. I couldn’t control energy. I couldn’t simply walk inside a building, much less go up the one flight of easy stairs to the 2nd floor. I couldn’t control people staring at me.
Memories ripped through my mind. I remembered people staring at me at McDonalds the first day I was discharged. I remembered how this lady approached me a few months ago on the lobby of the oncology waiting room to tell me “I was here that day they took you in the back in the wheelchair, you sure do look so much better now.” I know she meant well, but I found it shaming to be so bad off people could remember me months later. I thought about finances and how we were out of money, relying on the generosity of family to keep paying our house note. I was out of control on finances, having taken a 40% pay cut for disability. If it weren’t for the exceptional generosity of family, we would have had to declare bankruptcy. Medical bills were eating us alive. I remembered how I lost my bowels in public. The memories of endless time spent sitting or laying around feeling terrible was crushing me. All the lab draws, sometimes several a week when at home and daily at the hospital. I hadn’t been to work in 7 months and was wanting to simply be normal again. I felt anything but normal. All this stuff was flashing through my mind as the nurse handed me another cloth, the last one was now saturated with blood.
I felt the tears welling up. I really didn’t want to get upset, but could tell this was going to happen. It was deep, deep inside of me, a sorrow over what I had been reduced to. The tears started to pop out of my eyes. It wasn’t going to be a weeping ceremony, couldn’t get that lucky. This was deep from my gut and waves of emotion came spilling forth from my deepest innards. I hated it. I hated it. I did not want to be so upset. I cried and cried, trying to control the blood, trying to stop the tears. This poor nurse must have thought I was going to the looney bin. She was so kind. She offers another clean cloth. Between the tears and my now swollen eyes, I could see bruises on my arms increasing in size. Where did all these bruises on my legs come from? Mucous now mixed with the blood that was on the towels. It became even messier. I had no ability to control my body, my emotions, my future, my choices; I was along for a terrible nightmare that seemed it would not stop. It felt like gravity was getting stronger and my strength was fading. I could tell I was losing my battle and started to fear for my life at that moment in time.
The oncologist entered the room. He explained I was registering no platelets on the blood they had just drawn. He said my hematocrit was 6.9. He looked at me and said, “Mr. Baxter, you are very ill.” He examined the bruising across my scalp, arms, and legs and said I had to get blood right away. He explained he had already called the hospital floor and told them to prepare for my arrival and stated I would be a direct admit to the 7th floor. He said they are preparing transfusions on an emergency basis.
Two paramedics with a yellow gurney appeared at the door. I realized they wanted me on that blasted metal contraption. I thought about that long trek through the waiting room, how full it was, how I was an emotional bloody mess. They helped me onto the gurney and strapped me in. They tried to put oxygen on me, but it wasn’t going to work well with the bleeding. I was trying to hold the towels near my nose.
I asked the paramedics to take me out a back way….
there – is – no – back – way
Out through the same large waiting room filled with the same people staring at me. I had blood on the towel under my nose. I couldn’t stop the emotions from flowing and a new level of low became my reality. I wish I could tell you differently, but I felt so much shame, like I was a public spectacle. I knew no one meant it that way and no one asked for this, it just is. I was pushed through that large waiting area across to the elevator. I wanted to die.
About that time, fever and chills set in powerfully. I started shaking to the core of my body. Fever spiked and stayed between 101-103 for days, with small moments of reduced fever after a dose of Tylenol. My breathing became labored and they started breathing treatments. I learned I could shake from both albuterol treatments and from deep chills. It was two different kind of trembling. Chills were more in my bones and the albuterol made my muscles and skin tremble. It was miserable. I was sweating profusely and experiencing profound weakness unlike anything I had experienced up to that point. The nurse realized something else was wrong and made phone calls. Lots of blood was drawn. Soon, I had two doctors standing at my bed discussing various options, trying to troubleshoot what they could do. The x-ray revealed pneumonia. The talk was possibly removing my port, the most likely source of the infection. They discovered fluid around my heart.
August 27th, I wrote in a journal that they were wondering if my port was being rejected. They had all but ruled out infection, as they couldn’t get anything to grow on a culture at that point. The issue here is that my port is a double lumen port, not as common. It had been a major battle with the insurance company to get this inserted and cost several thousand out of my family’s pocket. If they remove it, the implications are terrible for me. I had recorded “I’m so weak that I can’t even open a soda can or bottled water. I tried to get up to go to the bathroom earlier and slid across the floor and sort of controlled crashed into the bathroom. They’ve put me on bed rest and turned on an alarm so that if I get out of bed, it squeals. My lungs started filling with fluid. Some steroids and breathing treatments have made a big difference there. My poor wife is getting worn down and the girls are getting concerned. The cancer is getting the best of me. I still have a 50/50 chance of making it. So far, it all points to the good 50%. But I’m so weak and sick right now.”
In a cruel twist of fate, something else happened that brings me to tears. My mother-in-law had visited with us a couple of times this year. She was a vibrant woman in her 80’s. She walked slow yet had a quick sharp wit about her. I recall a specific moment when she walked faster through the house than I did. We both had a good chuckle over that. My wife brought me terrible news in the midst of this hell I was in, just terrible news. Viola had fallen. She had slipped into a coma.
I began to worry something fierce about my wife. How in the world she could deal with all of this? She was now raising the kids, working full time, keeping the house together, helping me, and now her mom. My wife is resilient but everyone has a breaking point. I truly worried about her. I was worried about my future, if I was going to survive the next few weeks. I thought of my daughters, my family and friends. I couldn’t even get out of bed and I was getting very worried if I was going to make it. The weight of all of this pressed in deeply upon me and I said a prayer and gave up.
I was so exhausted. All I could do was lay in bed. I couldn’t even bathe myself. One night a patient care technician came into the room while I was on mandatory bed rest. She asked me when the last time was that I had gotten “cleaned up.” I wasn’t even sure. I was laying in a sweaty set of linens. I had called my sister and she was going to come up to help me, but hadn’t arrived yet. As the PCT left the room to get supplies, I felt humiliation at the idea that I couldn’t even bathe myself. I knew it was her job, but I had never been reduced to such a state in all my life. I was so sick, so weak, and so worried about my wife and myself. In comes the PCT with a stack of linen and bathing supplies. I tell you what, she was the consummate professional. She cleaned me from head to toe, changed the linens, and was out the door in 20 minutes. I felt so much better. I gave her a big “thank you.” He professionalism and compassion was not lost on me, it was inspiring.
I recorded the following on September 5th, 2008:
“Turns out my port in my chest isn’t infected. This is a good thing. Since I have been getting so low on my immune system, I had a type of virus called CMV activate in my body. Something like 80-90% of all people carry this virus. The immune system normally keeps this relatively harmless virus under check. Not me. Since I’ve had my immune system (white blood cells) go down to 0 twice in the last two months, this virus has decided to play around with me.
They did a CT of the chest and abdomen and didn’t find any swollen lymph nodes, but did find evidence of very small pockets of “infiltrates”, which is basically pneumonia. That would explain the lung junk and coughing. I also have a “tiny pericardial effusion” which basically means a small amount of fluid around the heart. Both are treatable.
I’ve now been in the hospital for two weeks related to this illness. I was home for a few days before that. Suffice it to say I now almost live at the hospital with just short breaks at home.
I’ve been waking up each night in tremendous sweats. Sometimes once a night, sometimes 3-4 times a night. Since my wife’s mom has taken seriously ill (she fell, broke a hip, and is now unconscious), I called my oldest sister to come up and stay a while and help me at the hospital. I couldn’t have asked for a better nurse to fetch food, change soaked linens, and that kind of thing.
I still have a while to go before I’m allowed to go home from this illness. I can’t seem to get a straight answer out of the doctors. Then I will need a period of time to allow my body to build up some strength for the last round of chemo. Each round had knocked me down further and harder. Truthfully, I’m a bit scared of this last round and how terrible I will feel. I’m also starting to deal with something that I don’t normal deal with: depression. After my sister left today, the room was painfully quiet. Things don’t change from day to day anymore, I feel terrible everyday, it is lonely in here, and I guess I finally reached a point where I’ve just snapped.”
The two doctors appeared again at my bedside and shared with me about the CMV infection. Twenty one days of gancyclovir infusions. I was also told something that freaked me out in fresh, new, and exciting ways. They explained that CMV can attack the retinas of the eyes. There was a very real chance I might go blind. They said it was a maybe, maybe not deal, they had no idea of the chances. They clearly stated they felt they owed it to me to know how serious this was and to tell me of this dire possibility. Words cannot describe how empty I felt at that moment. I thought I had hit a low before, but the idea of going blind was more than I can take. That is when I snapped and broke. I thought I had given up before but this was more than I could stand to hear. I was a broken man. I had no man cards left to lose.
My wife brought a walker up and sat it next to the bed. First time up, I had two people, one on either side. I want to think my wife was one of them. It was a struggle to get to the bathroom. Felt so good to get out of the bed. I was amazed at how little strength I had, but pleased I was getting to try. Oh my gosh, I got to have a shower. It was so amazing to feel warm water running across my skin!
Several weeks later I was released from the hospital, improved but weak. I still had my vision! I can’t explain how much of a weight that was lifted off my shoulders. My mother-in-law had come out of the coma. I was told she was conscious but was jumbling words. My wife told me she was asking about me and was really concerned. We all were relieved she was able to think that clearly. I practiced walking. I would walk around the house. I eventually took two walks outside. The first one I didn’t go far. I had trouble walking without weaving around like a drunk man. I literally could not walk in a straight line and had trouble staying on the side walk. The second time I made it around the block. I was exhausted, but I did it!
Then rest of September 2008 proved eventful. I realized my driver’s license was expiring at the end of September. I felt this determination to make the trip myself. I mean, I can get there and back if I have a full day to do this. I look back and realize I was stubborn to have done this myself, but this sense of pride or whatever pushed me to make this journey, to focus on what I can do. I gained strength each day, just a tad. I celebrated my 44th birthday. I think this was the birthday I tried to cook homemade pizza and set the oven on fire. Oh boy.
I will never forget my trip to the department of motor vehicles (DMV). It was surreal. This swollen, bald man got up very early. After my loss of independence this last time around in the hospital, I was stubborn as a mule. I was determined I had to drive, had to push forward. I planned the day, arranged food, and medications, and started out with a bang. No, rather, a slow shuffle to the car. I was tired but knew the regimen to press on. The drive was long and the traffic bad, but I persisted. I got there early, about 15 minutes before the doors opened, so that I would not have to stand in a long line. I drove into the parking lot and saw a line of people already at the locked front doors. Oh my. I joined them. I stood in a line of people and actually felt a bit OK, tired yet gratified I was able to make it. When we got inside and took our numbers, I realized the sensation of overwhelming fatigue was setting deeply yet again into my bones. I leaned up against a wall and closed my eyes. The sounds and buzz around me was not helping me. Then it began. I felt both eardrums pull inward with sudden pressure, then released. No, not now, please. The pounder began and I heard the next number called for service. It wasn’t mine. I wanted to leave, but knew I didn’t have a choice. I had waited too long. I simply leaned against the wall, ignoring everyone around me, making sure that wall did not fall over. No chairs were available for me to sit in. Next number was called, I inched forward, following the line. Finally my number was called. I didn’t want a new photograph taken, but it had been 12 years and I had no choice. The lady reassured me that I could get another one done. I was very sick looking, ill as can be, pale, swollen, had this knot on my head (Ommaya), weak, and my head was pounding. I hated the flash of that camera. I hated the idea of having a picture like this on my driver’s license. I hated how I felt. I left hating that moment. I hated it. I hated my life and what it had become. Now I was having this memorialized on my formal ID almost like a cruel joke. I determined I would get a new picture as soon as I felt a bit better and looked better. I can’t recall the drive home. That scares me.
I had to get back to the oncologist’s office weekly for blood testing. I needed my last round of chemo. My blood counts remained low, too low to start chemo. Each time I went, I was expecting to be admitted for my final treatment. I had all my hospital stuff in my car, pink sign for the door included. I was told to wait one more week. This happened every trip.
By mid-October, it had been about 8 weeks since my last dose. I felt my time was up for chemo. I spoke with my wife. I called my mom and stepdad. I spoke with a few others. My body was not recovering. For better or worse, I withdrew from the entire deal. I called my oncologist and spoke with the RN for over an hour. She tried to talk me out of quitting. I held my ground. She used the phrase repeatedly “but you’re an RN, you should know these things.” She assumed I knew everything about cancer, oncology, the moon, weather patterns of the Earth, you name it. She pissed me off. I was the patient, not an RN. I was sick and not at my normal mental capacity. I was getting angrier by the moment and finally set the record straight and told her to back off. I finally ended the conversation by saying it is my life and I’ll take my chances, I can’t take anymore. It is now the middle of October. My last dose of chemo was in the summer and my body is tired and is clearly indicating it can’t take any more. I took back control of my life and told them to leave me alone. I would be in next week to get cleared to go back to work. Thank you, have a nice day. I’m through. Enough!
I triumphantly returned to work on October 16th, 2008! I was so happy! I remember walking into the office and coming around the corner to my classroom. I could hear the substitute RN talking with the students. I introduced myself. It felt amazing to be back!
I want to shift gears for a moment. I have something deep and personal I feel I must get off my chest. This next part is hard to share, hard to relive, but I must. I received so much love. I discovered relationships matter more than anything in life. Humans are of the highest value and relationships are the highest expression of that value. I was capable of valuing relationships more personally and intimately than ever before. I was acutely aware now of how much I was loved. I was able to look back at an eight month nightmare and see so much love shown to me.
Why is this so hard to share, you might ask? I was incapable of returning the very love I was shown. I felt the love, received the love, and could not return the love.
Chemotherapy and stage IVb cancer stripped me of so much and showed me how weak I really am. The stark contrast between inability to do right, while being loved overtly by so many, was almost more than I could withstand. I was incapable of controlling my emotions. This was exceptionally difficult for me and I felt less a man, a poor father, and a lousy husband. I could be kind one moment, mean the next. I was filled with hope for a few hours, followed by stark realities that my time on this Earth might be cut short. Long stretches of time in the hospital stole so much of my dignity. My daughters were busy with school yet having to face the reality of a dad who was quite sick.
I was no joy to be around yet tried so hard to be an example of bravery. My wife worked a full time job and tended to the family, house, bills, coming to the hospital, driving me around on her days off, and towards the end, her mother entering into a coma for several days. She did it all and did it willingly. I couldn’t have possibly asked for more from her. I regret to say I was incapable of returning the love.
Family, friends, and so many rallied to help us keep our household operating and sustained us so we didn’t lose the house. Getting a card from the family reunion with so many who signed it overwhelmed me. Getting a call from a niece on a weekend night to tell me they had just raised thousands of dollars 9 hours away in South Texas reduced me to a bowl of jelly. We were needing help with the van to keep it running and I was able to get the necessary repairs. Mom and Jim gave until it hurt to keep us from losing our house, to help pay over $2,000 for the port in my chest, sacrificed so much time and money to travel to help. Janice’s family cooked, cleaned, took the girls shopping for school clothes, bought them cell phones, helped Janice with emotional support, and gave so generously. Friends brought me movies to watch, lifted my spirits, brought me burgers and munchies and treated me so kindly. The profound highs and lows took their toll yet I was so grateful for all the love and generosity. Everyone was simply amazing and family close and far rallied to help in every way imaginable. I hope I didn’t forget anyone, please forgive me if I did.
So what is so hard about all this you might ask? From the outside world, I was given the welcome of a hero. I was treated like a king. People went the extra mile for me and my family. It is natural to encourage a cancer victim and help them make it to the next day. We all want a cancer patient to survive. I received many compliments and was told innumerable times how brave I was, how good I was doing, and people would say some variation of the following to me: “if I were in your shoes, I wouldn’t be doing so well.”
If only they knew the truth how I really felt inside. I’m going to tell it as I recall it and I assure you, I remember well. The world saw one thing and heaped praises; my family saw another side of me and loved me unconditionally during my volatile swings. Burkitt’s Lymphoma and aggressive chemotherapy made me sick. I was not well. I was not well physically, mentally, or emotionally. I was not pleasant around my wife and daughters when the outside world wasn’t looking on. I can honestly say my inability to return the love shown to me is my greatest regret. My desire to be sweet to my family was strong, yet my inability to fulfill this desire just about killed me. I could have at least been kind, or quiet. Instead, I was an angry man on the inside and outside when the world was not looking on. I was filled with so many contrasting emotions that I was difficult to be around. Yet I was treated as a hero.
I regret I did not treat my family as kind as they treated me. I witnessed the true definition of grace: undeserved favor. It is one thing to have a bad moment here and there, but I was difficult more than not. I did not deserve the kindness I was shown; they returned to my side to help me day in and day out. My wife and daughters put up with me and I assure you it was most difficult on them.
Want to know the hardest part? I was a man who was fully aware of what he was doing, but was incapable of doing better. Just as I couldn’t control sleep, control medical appointments, stop bruising, couldn’t make my own decisions, and stop strange discharges out of bodily orifices in public places, I could not control my emotions and outlook in private. I tried, trust me, I tried. I tried and I tried. I failed so many times and was a man trapped in a body that was not his to navigate physically and emotionally. The torment of knowing what I should have done while being pushed beyond my ability to contribute meaningfully to my own surroundings in a positive way was perhaps the single greatest heartbreak for me. My family deserved better and I feel that I failed them. I did not fail them by choice as much as circumstance. What others saw as a hero, they saw an angry sick father and husband. I have made peace with this as I realize I was not in control of much of anything. My lack of control does not stop how bad I felt over how I treated them.
I salute my wife Janice and my daughters Andrietta and Chauncey for being so patient with me, extending to me the very kindness and grace I did not possess to return back to them. I love you all the more for your grace and kindness. You cannot know how remaining at my side during that time and the recovery period the last few years have meant to me. I will never be able to fully repay you, but intend to do my best to be there for you in your times of need.
You might ask, why would you share something so personal Robert? I’ll tell you why. I hope my words can help some others to have as much grace with their family members who are going through devastating illness. I seriously doubt I am the only one who has gone through such a stark contrast: hero to the world, difficult to my family. If my words can shed light on the private hell that families go through, it is worth the disclosure. We all want to keep a brave face. I’m sure some do better than others with kindness. Deep behind tragic illness is a family stretched, pushed to their limits, and flailing about to recover after it is all over. What the world doesn’t see because no family really wants to share it, is the power of a sick family member to bring an entire family to its knees. We keep a brave face for the outside, try our best to not fall apart in private. The daily wear and tear of having a loved one so sick is beyond demanding and pushes every person in the household to the brink of their limits.
I am an active member of the Burkitt’s Lymphoma Society. We have an active private forum for caregivers and those who have had Burkitt’s to help those suffering with this powerful cancer. We have grown close as a group. We share. Trust me, what I have shared is something experienced by other families. Such overwhelming long term illnesses push any family to the brink of their strength, sometimes families break apart. Sometimes they rally closer. Either way, it is so difficult and the inside members get to see everyone at their best and worst. Now that this disclosure is over for the moment, let’s resume normal programming content.
As Paul Harvey would say, “Now for the rest of the story.”
When I returned to work, I had one major surprise waiting for me that was truly unexpected. I sat in my office and the chair was not my chair. I couldn’t believe how hard the chair had become; I felt I was sitting on metal. I could not believe someone had switched my original comfy office chair for some tired used piece of nothing. This one had no cushion in the seat! It was nothing but metal. A fellow I worked with brought bubble wrap from the back and it made a cushy soft place to sit. I spoke to the secretary in the office next to mine. She assured me that was the same chair. Turns out I was the one with no cushion in the seat, not the chair.
Not long after I returned, the same secretary shared with me about being a lifetime donor for Carter Blood Care. She gave platelets and blood as regularly as they would allow. She had done this for years and is a lifetime donor. She mentioned she had asked Carter to check if her blood was a match with mine. It was. She explained that she was the primary donor of platelets and blood, straight from her to me.
It took a moment to sink in. The lady who worked next to me had been supplying my blood needs this whole time! There went another man card. I wept and gave her a big hug.
Please give the gift of life!
Life is a trippy adventure now. Recovery from so many long months of chemo and aggressive cancer was not what I expected. I am a man of gratitude most of the time. I can work. I can drive. I can still do things around the house. I have regained control of most of my body. But I have not returned to the old Robert. I have had to grieve over losing my old self. I am not the same man. I wish I could say “I’m a better man.” I suppose that is true in some ways, but physically, nothing could be further from the truth.
I am still working on accepting “The New Me.” Due to the severity of the cancer and the chemotherapy, I have had ongoing challenges. I could go on with a list of what I deal with now, but let’s suffice it to say I am grateful to God to be alive, to be working, and to have another day to extend the kindness, grace, and mercy shown me. I do not measure up to the standard I would like physically. I take life at a much slower pace, being careful to measure out my limited energy.
Not every day is easy. When I have some really down moments, I reach back and recall there was a day when all I wanted was to get out of that hospital bed and return to work. I open my wallet and look at my drivers license picture and stare at the bald swollen hairless man.
The picture on my driver’s license has not changed. I now keep it in my billfold proudly as a token, a memory, of a day when I simply wanted to be able to work again and leave behind the torment that is cancer.
I still have the pink sign that hung on my hospital door for nearly 8 months. I got it laminated and will keep it forever. I still have the superman shirt, the Ommaya reservoir tube (yes the surgeon gave me one!), and scars on my physical body. The headaches slowly left and I haven’t had a good ear popper in a while.
Life after Burkitt’s is not what I thought it would be. I thought that once cancer was over, it was over and done with. Either I lived or didn’t. That isn’t true in my case and many like me. I am filled with gratitude that I did not have before cancer. Relationships matter so much now. Petty small things seem more just like that: petty. I see life through a new lens of how prevalent suffering is in this world. I find I can cry at the drop of a hat. I do not have the energy I once did. I don’t take work and the ability to work for granted. I have to be so careful now about infections and doctor visits. I have learned how expensive health care is and how much good health is really worth. Smallest acts of kindness can have lasting impact. There are some really good people in the world.
I think I would have to end on the topic of love. I set out in 1999 as an intentional life pursuit to fulfill the greatest commandment: Love the Lord your God with all your heart, soul, mind, and strength. Love your neighbor as self. I would have never thought that something as devastating as cancer could teach me so much about love. I initially felt I had been dealt a very unloving situation. Maybe that isn’t true when I consider the depths of what keep coming to my life these days. Love has increased so much for me, conscious love. Cancer began a powerful search for what a makes a difference in this life, in my life, in others lives. I find I have an increasing grace to offer others that wasn’t present before. All of this challenges me to not be indifferent, to make a difference, to extend love where I might not have before.
I suppose I do have more strength than I realized.
|
|
|
Submitted by: Robert Baxter |